Brachial Plexus injuries can greatly lower the quality of life for people suffering from it. For example, synaptic networks of nerve fibers from various spinal or pairs of spinal nerves (plexuses) may be damaged due to injury, accidents, tumors, pockets of blood (hematomas), or autoimmune adverse reactions. Pain, weakness, and loss of sensation may also occur in all or in some parts of the arm or leg.
Electromyography and nerve conduction studies help doctors locate the damage, and an MRI or CT scan helps determine the cause. Sometimes treating the disorder that’s causing the problem restores or improves neurological functions.
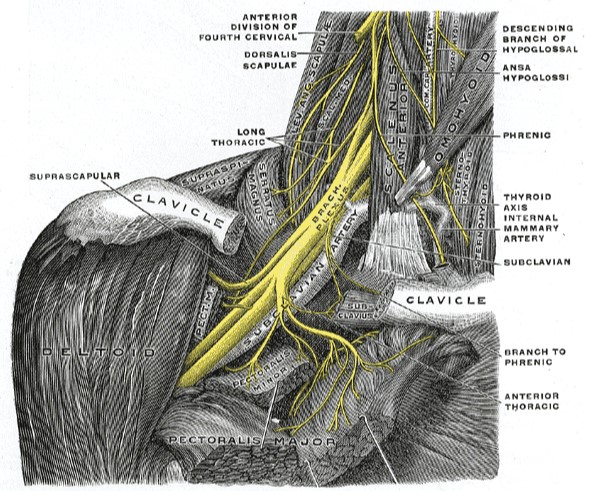
A plexus is like an electrical wiring box that distributes wires to different parts of the house. In a plexus, the nerve fibers from different spinal nerves (which connect the brain and spinal cord to the rest of the body) are sorted out so that all the fibers going to a specific part of the body are put into one nerve.
Extreme damage to the nerves in the greater plexus region can cause problems in the arms or legs that these nerves support.
The main Plexi are:
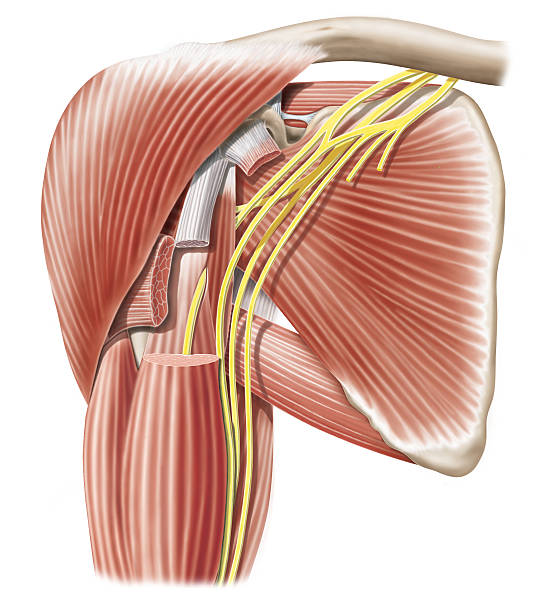
- The brachial plexus, located in the neck and shoulders, distributes nerves to the arms
- The lumbosacral plexus, which distributes nerves to the pelvis and legs
The lumbosacral plexus consists of:
- Lumbar plexus in the lower back
- The sacral plexus in the pelvis
Neurotransmitter boxes for the body: The plexuses
A plexus is like an electrical wiring box that distributes wires to a home. In a plexus, the nerve impulses and fibers from the different spinal nerves are grouped and regrouped, so that all the fibers going to a specific part of the body are put into a single nerve.
There are four nerve plexuses in the body frame:
- The cervical plexus: Providing nerve connections to the head, neck, and shoulder.
- The brachial plexus: Providing nerve connections to the chest, shoulders, arms, forearms, and hands.
- Lumbar plexus: Providing nerve connections to the back, abdomen, groin, thighs, knees and calves.
- The sacral plexus: Providing nerve connections to the pelvis, buttocks, genitals, thighs, calves, and feet.
How can the brachial plexus be injured?
The most common causes of damage to the Plexi are:
- Physical injury
- Cancer
- An injury or an accident that dislocates or severely twists the arm at the shoulder may damage the brachial plexus (located near the shoulder). The brachial plexus can be damaged during delivery in newborns if the delivery requires pulling or other maneuvers. Falls can also result in injury to the lumbosacral plexus (located near the hip).
- Cancer that grows in the breast or upper part of the lung can invade and destroy the brachial plexus. Cancer of the intestine, bladder, or prostate can invade the lumbosacral plexus. Other masses, such as a noncancerous (benign) tumor, abscess, or pocket of blood (hematoma) may cause ), perturbations of curls by squeezing them.
- Diabetes or radiation therapy for breast cancer, which can damage nerves throughout the body, may also damage the nerves in the plexus.
- Acute brachial neuritis (Parsonage-Turner syndrome or painful muscular dystrophy) is sudden dysfunction of the brachial plexus due to inflammation, not injury or cancer. It may be caused by an autoimmune reaction when the body produces antibodies that attack its own tissues. This disorder mainly affects men. It usually affects young people, but it can occur at any age.
Symptoms of brachial plexus
Dysfunction of the brachial plexus causes pain, weakness, and loss of sensation in the arm. All or part of the upper extremity (such as the forearm or biceps) may be involved. If the cause is an injury, recovery tends to be slow over several months. Severe permanent weakness.
Acute brachial neuritis causes severe pain in the arms and shoulders. The arm usually becomes weak, and reflexes are disturbed as the pain subsides. Patients may be unable to form an “O” shape using the thumb and forefinger. The weakness subsides within 3 to 10 days, and patients usually regain strength within the next few months.
Dysfunction of the lumbosacral plexus causes pain in the lower back and leg, as well as weakness and loss of sensation in all or part of the leg (such as the foot or calf). The chance of recovery varies with the cause of the condition.
How to diagnose brachial plexus
Electromyography and nerve conduction studies
Magnetic resonance imaging or computed tomography
Doctors suspect a plexus infection when symptoms gather in a part of the body innervated by this plexus. The location of symptoms indicates the affected plexus.
Electromyography and nerve conduction studies can also help locate the damage.
An MRI or CT scan may help determine whether cancer, another mass, or an injury is causing a plexus disorder.
Treatment of brachial plexus
- Treating the cause
- Pain relief
- Sometimes physical and occupational therapy
The specific treatment of polyneuropathy varies with the cause, as follows:
- Diabetes: Careful control of blood sugar levels can slow the progression of the disorder and sometimes relieve symptoms. Sometimes a transplant of islet cells (cells that produce insulin), located in the pancreas, cures diabetes, alleviating neuropathy.
- Multiple myeloma, liver failure, or kidney failure: Treating these disorders can lead to a slow recovery.
- Cancer: Surgical removal of cancer may relieve the symptoms.
- Hypothyroidism: Thyroid hormone is administered to the patient.
- Autoimmune disorders: Treatments include plasma exchange (filtering toxic substances, including abnormal antibodies from the blood), immunoglobulin (a solution containing many different antibodies collected from a pool of donors) intravenously, corticosteroids, and drugs that inhibit The immune system (immunosuppressants).
- Drugs and toxins: Sometimes stopping drugs or avoiding exposure to toxins can cure neuropathy. Antidotes are available for some drugs and toxins that can correct some of the toxic effects.
- Excessive amounts of vitamin B6: if the use of the vitamin is stopped, the neuropathy may resolve;
- If the cause can’t be fixed, treatment focuses on relieving pain and problems with muscle weakness. Sometimes physical therapy reduces muscle stiffness and can prevent contractures. Physical and occupational therapists can recommend helpful assistive devices.
- These include the antidepressant amitriptyline and the two anticonvulsants gabapentin and pregabalin, and mexiletine (used to treat arrhythmias). In the form of a lotion, ointment, or skin patch.
Know more about the brachial plexus from Dr. Burak Sercan.
Dr. Burak Sercan will answer all of your questions about TOS and how to prevent, treat, and live with it.
Our specialized team of specialists in Turkey can help you with all the inquiries you have about brachial plexus surgery. Contact us now to know more about your next procedure.